Understanding Persistent Dizziness
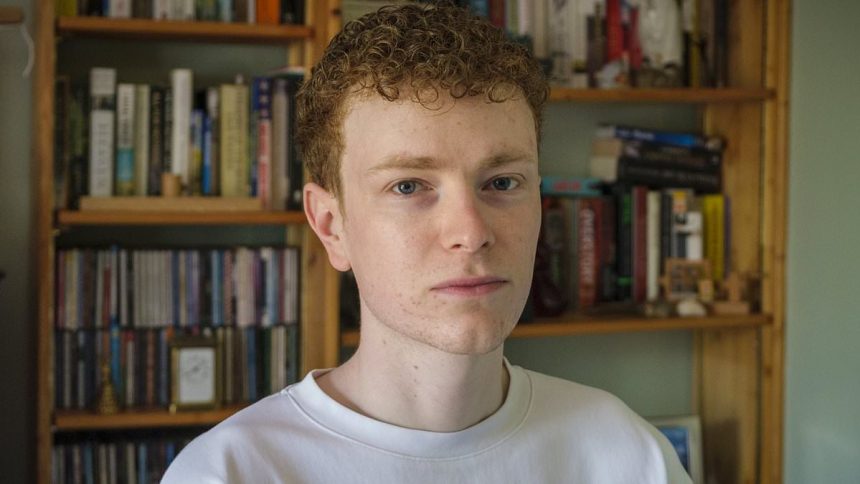
Cameron Hathaway, a 27-year-old physiotherapist from Leeds, has long been familiar with the dizzy spells triggered by his migraines. However, last summer, he experienced a new sensation: a disorienting ‘rocking’ feeling that lingered well after his migraines had subsided.
“I had a spinning feeling during the migraine, but what followed was more of a rocking motion – everything around me was moving,” Cameron explained. This sensation, once short-lived, morphed into a persistent sense of unsteadiness that began to impact his daily life significantly.
Seeking Answers
Fearing a brain tumor, Cameron first consulted a general practitioner who attributed his dizziness to migraines, even in the absence of other typical migraine symptoms like headaches. To alleviate his concerns, another physician scheduled an MRI, which dismissed any tumor fears. However, Cameron’s struggles only intensified. His attempts to maintain balance led to severe eye strain, making reading and travel difficult.
“I had to stop work because I need to read for my job,” he lamented. His previously active lifestyle dwindled as he limited outings to only brief walks.
Finding the Right Diagnosis
Over the next six months, Cameron consulted two neurologists, both insisting his symptoms stemmed from chronic migraines. While one recommended lifestyle changes to avoid migraine triggers, the other prescribed beta-blockers to manage anxiety. Regrettably, these measures failed to alleviate his symptoms, prompting Cameron to seek help privately.
In April, he visited Dr. Diego Kaski, a neurologist at the National Hospital of Neurology and Neurosurgery in London, who specializes in balance disorders. Dr. Kaski diagnosed Cameron with Persistent Postural-Perceptual Disorder (PPPD), also known as 3PD.
“It is one of the most common conditions that balance specialists see – it’s just that many GPs and emergency physicians are unfamiliar with it,” Dr. Kaski noted.
The Nature of PPPD
Though the symptoms have been recognized for years, 3PD was only classified as a neurological disorder in 2017. It typically follows inner-ear balance issues or can stem from incidents like concussions. This disorder causes chronic dizziness with a ceaseless feeling of unsteadiness.
“When something – like an inner-ear problem – causes dizziness, the brain goes into hypervigilant mode,” Dr. Kaski explained. As the brain relies increasingly on visual cues to maintain balance, it misinterprets sensory information, resulting in a constant feeling of dizziness in busy or visually stimulating environments.
This condition often creates a self-perpetuating cycle of anxiety and avoidance, exacerbating symptoms in those affected.
Recalibrating the Brain
Dr. Kaski compared PPPD to a software issue on a computer, stating, “The hardware [receptors in the ears, eyes, and feet] are all working, but the software [brain processing] is malfunctioning.” To regain balance, treatment typically involves gradual exposure to movements or settings that trigger dizziness, a technique known as vestibular rehabilitation.
Cameron recalled the challenges of facing his triggers: “Something that involved standing still, such as washing up, was difficult. So, as Dr. Kaski instructed, I exposed myself to this trigger – initially spending a minute or two washing up, and then building it up so I could do it for longer and longer.”
Since anxiety frequently compounds PPPD, techniques to promote mindfulness can help manage symptoms. Debbie Cane, an audiologist at Withington Community Hospital, noted the importance of being aware of one’s breathing and taking regular breaks from activities to avoid tension.
Progress and Hope
Cameron found the diagnosis transformative: “A big part of my treatment was awareness that my brain was over-sensitive to motion around me, and to learn not to be afraid of 3PD symptoms. The diagnosis helped me to calm down, and consequently my 3PD symptoms improved.”
He implemented strategies to manage his migraines, including staying hydrated and reducing stress.
“Over time, things have improved – I would say I’m about 70 percent recovered now,” Cameron shared. Having regained the ability to read for longer periods, he’s hopeful about returning to work soon.